Renda was participating in an Aug. 7 webinar, hosted by David Nace, M.D., chief medical officer of health data insights platform vendor Innovacer, that also included David B. Nash, M.D., M.B.A., founding dean emeritus of the College of Population Health at Thomas Jefferson University in Philadelphia, the first college of population health in the country when it was founded 10 years ago.
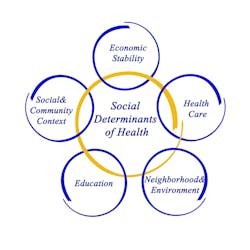
Drs. Renda and Nash joined Dr. Nace in a discussion of how providers and payers are redefining population health management with social determinants of health.
Looking back 10 years, Nash said initially there was a growing recognition that population health is not just about delivering health services, it is about what makes us healthy. “Ten years ago, most folks were just trying to understand what make people healthy,” he said. “The sad conclusion was that it was not the delivery of healthcare services; it was everything but that. Having been inside Jefferson for 30 years, imagine how we felt when we figured out it wasn’t about us. The delivery system is an important part, but 80 percent of the story has nothing to do with what we do at the bedside.”
Nace reminded Nash that he had helped coin the phrase “No outcome, no income,” as a nod to the rise of value-based payment. Nash said that phrase is about going upstream to shut off the faucet instead of mopping the floor. In other words, payers are starting to look at ways to focus on what is causing people to need surgery instead of encouraging providers to build more bariatric surgery centers.
Humana’s Renda spoke about how several years ago the insurer set a goal of improving the health of its members by 20 percent by 2020. The first step was to determine what they meant by making the population 20 percent healthier. They settled on using a CDC Healthy Days survey tool, which gives equal weight to mental and physical health. It simply asks people how many days they were physically or mentally unhealthy in the last 30. “Everything we did cascaded from that,” Renda said. “We have used that in a number of ways, including as a surveillance tool across different lines of business to understand the base line of unhealthy days.”
With its efforts to address food insecurity or diabetes, Healthy Days is a leading indicator. Humana executives can watch trends in the numbers to see if interventions make a difference.
As the insurer expands to Medicaid coverage, it uses the tool to learn about new members’ health status. “Anyone who reports over 20 unhealthy days gets a warm transfer with a health navigator or triage to community or clinical resource,” Renda explained. “It has been a great tool for us.”
Renda says social determinants such as food insecurity and loneliness turn out to be the biggest drivers of unhealthy days, rather than traditional clinical diagnoses of chronic conditions. “That has generated insights and helped us focus our work,” he added. Humana built its analytic and intervention pipelines around both. Research shows that people who are food insecure are more likely to be diabetic and have chronic heart failure.
When someone has isolation and loneliness, it leads to depression and dementia, Nash added. To tackle loneliness, you need community centers and transportation. Connecting all these dots is a lot of hard work on the ground, he said.
Renda agreed that tackling an issue such as loneliness is difficult. Humana has worked with an organization called Papa Pal, which hires college students to spend time with older people, watching a movie or helping them pick up prescriptions. He said in an early study, just doing it 10 hours a month for four months reduced the loneliness scores significantly in the Unhealthy Days survey.
“We know when you tackle the social determinants, there are savings on a per-member per-month basis,” Nash added. “Payers have economic incentives aligned to tackle social determinants. There is margin to be made by improving the social determinants. When people have fewer days of loneliness or depression, they decrease utilization. There is great data being assembled in places like Humana and elsewhere.”
Nevertheless, Nash said, providers still have lots of questions about bridging gaps between clinical and social needs. If you gather social determinant data from patients, where does it go, who gets to see it, and how do they get actionable information?
Most provider organizations are just starting to explore this idea and putting their toes in the water, Nash added. “I think many practitioners find this difficult. They weren’t trained this way — to ask patients whether they have adequate transportation. For many primary care doctors, this is all radical new stuff. Most organizations are just getting their arms around it. It will be stimulated by changes in reimbursement. Making it economically viable is where we have to go. I am excited about the Oncology Care Model, CPC Plus and a new agreement between Blue Cross/Blue Shield of Minnesota and Minnesota primary care practices. We are going to see more collaboration between payers and providers on more exciting models.”
Renda agreed that a lot of physicians weren’t trained to think this way, and don’t know where to send a patient if they say they are food insecure. “There are education, technology, and intervention pieces that need to be addressed,” he said, adding that health systems and payers need to elevate social determinants to the level of clinical gaps in care. “For condition like diabetes, in addition to medications and screenings, you check about transportation and whether there is food in the refrigerator,” he said. “Treat them as the gaps as they are.” Another issue, he said, is that the healthcare sector has to develop some common definitions of social determinant data elements.
“Humana is all in on this. We are committed to addressing social determinants, but the proof is in the pudding, Renda said. “We need to generate clinical outcomes and a business case that shows that by addressing them, we are keeping people out of the hospital and lowering the total cost of care.”
These efforts are always going to cost money up front, Renda noted. “The challenge for us is that the further upstream you go, the longer it takes to see return on investment. I don’t think these patients are going to cost more in the long run, but we have to open the aperture a bit. We can’t think we need one-year return on investment. It may take three years, five years or longer. The payoff may come further down the road.”