As the world remains laser-focused on the COVID-19 pandemic, the nation’s opioid epidemic continues to loom in the background. Between 1999 and 2014, drug overdoses nearly tripled, and almost 450,000 people died from an opioid overdose. In 2017, the U.S. Department of Health and Human Services declared the opioid crisis to be a public emergency.
Despite the attention government officials and the medical profession have placed on the opioid crisis, usage is increasing. An aspect of opioid addiction that requires more attention is the tie to surgical procedures. Research shows that 7% of adult surgical patients and 5% of adolescent patients develop persistent opioid use following surgery. Given that more than 50 million surgical procedures are performed annually, surgery represents a major gateway to opioid addiction, potentially causing harm to more than 2 million surgical patients each year.
This crisis, coupled with an opioid shortage, spurred anesthesiologists at Seattle Children's Hospital and its Bellevue Clinic and Surgery Center (BCSC) to undertake a quality improvement initiative to decrease the use of opioids. We assembled an interdisciplinary project team to focus on reducing the use of opioids during surgery that was charged with adding value to our clinical services by maintaining or improving surgery outcomes while reducing costs.
The BCSC quality improvement project began in January 2018. Initially, our clinicians focused on reducing the use of opioids in pediatric tonsillectomies, which have historically relied on the intraoperative administration of opioids for pain management. Using MDmetrix, an artificial intelligence (AI)-powered analytics platform, our team analyzed more than 10,700 surgical cases across many different clinical approaches, re-evaluating medications that had been long been considered “standard practice.” Next, we devised a series of pain management protocols, based on published research. We also followed the Plan-Do-Study-Act (PDSA) cycle, which is a standard methodology for the development of clinical improvements using real-world data.
Whereas previous PDSA improvement cycles had been measured in years, our team was able to leverage AI to complete improvement cycles in just 12 weeks. Utilizing real-world data routinely collected in our electronic medical record (EMR), our team monitored and evaluated the comparative effectiveness of our current and historical protocols on an ongoing basis. As a result, we were able to quickly adapt our protocols, incorporating evidence-based best practices, to effectively manage surgical pain while reducing patients’ opioid exposure.
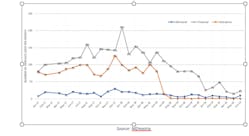
Following this initial success, we expanded our approach to include other surgeries across a range of disciplines, including orthopedics, urology, plastics, dental, ophthalmology and general surgery. The results were groundbreaking. We developed protocols that eliminated the use of opioids during surgery from the vast majority of our outpatient procedures (dropping from 84% to 8% of procedures), while also reducing the need for postoperative morphine administration from 11% to just 6%. To date, more than 6,000 patients have now successfully undergone surgery at BCSC without opioid administration.
With these opioid-sparing protocols, our clinicians found that postoperative nausea and vomiting—the most common side effect of anesthesia, caused by opioids—virtually disappeared, while pain scores, total anesthesia time, and total post-anesthesia care unit (PACU) time remained stable. Overall, costs also decreased (85% reduction in cost for analgesic medications), while patient/parent satisfaction increased dramatically.
This transformative opioid-reduction work represents a paradigm shift in how clinicians can improve clinical outcomes, shifting the all-too-common multi-year lag between “bench discovery” to “bedside care” to just weeks or months. Over the past decade, hospitals have heavily invested in EMR technology to capture digitized patient data, with the U.S. spending over $40 billion in federal funds to support EMR implementation. Yet, the United States has so far seen little return on that EMR investment in terms of reduced cost or improved outcomes. This case study powerfully demonstrates how the healthcare industry can leverage digitized data to improve patient care, patient safety and operational efficiency.
Dr. Latham is a pediatric anesthesiologist and director of pediatric cardiac anesthesiology at Seattle Children's Hospital and has authored many publications on advances in anesthesiology and healthcare improvement. He also serves as an associate professor of Anesthesiology and Pain Medicine at University of Washington. Dr. Latham earned his MD at the University of Kansas.