Enterprise image management (EIM) applications have been receiving greater attention lately, but how real is it? Differing perceptions and definitions complicate a clear understanding of the realities of enterprise image management. This discussion is meant to provide some clarity on the subject, and to suggest an approach to the development and implementation of an enterprise image management strategy.
Definition
Part of the reality of EIM is the variation in its definition. There is lack of a consistent definition of what is meant by enterprise image management, and consequently there is confusion in trying to assess the extent of its implementation. Perhaps the most comprehensive definition can be found in the HIMSS-SIIM White Paper
In its simplest form, EIM might represent a common image management infrastructure within a single provider facility that addresses more than one service line where clinical images play a key role in the daily workflow. This could be as simple as a shared vendor neutral archive (VNA) between radiology and cardiology service lines, along with a common image viewer.
A true EIM might be expanded to cover multiple provider facilities, span multiple image management applications, and potentially multiple IT infrastructures in those facilities to provide a common image management and viewing environment. In addition, such a solution would need a patient-centric driven workflow and interoperate with a number of different systems, including electronic health record (EHR) systems, clinical decision support (CDS) systems, artificial intelligence (AI) systems, as well as other clinical digital imaging systems used in specialties such as GI, dermoscopy, pathology, etc..
In reality, most implementations today are more likely to be akin to the first example as opposed to the latter. Part of the reality is how well these initial implementations may scale to address the needs of a growing enterprise, such as a growing integrated delivery network (IDN).
Drivers
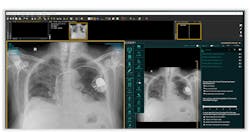
Image management and accessibility more than likely will vary by service line. For example, in radiology, the primary purpose of an image management solution is to clinically present relevant images to a diagnostician for interpretation. Secondarily, images may be accessed by other clinicians such as neurosurgeons or orthopedic surgeons who need access to images for surgical planning. General clinical access to images may be required, such as in the case of assessing chest tube placement, and lung function status.
Cardiovascular care is similar, but can be divided into two categories, those being interventional and non-interventional. In the case of interventional, images are assessed as part of a therapeutic process such as percutaneous coronary intervention (PCI) procedures. Non-interventional procedures may be more akin to radiology, wherein images are acquired and interpreted by a cardiologist, as in the case of echo sonography or ECG procedures.
Some images are acquired, and not necessarily retained as with point-of-care ultrasound (POCUS) in the emergency room (ER). These types of procedures have classically been for guidance or observation purposes, and they have not been viewed as clinically significant for retention. Additionally, such procedures follow an encounter-based workflow, where no procedure order is created.
In other services such as dermatology, or orthopedic practices, images may be acquired simply to document or follow treatment progress. Such images may or may not have been retained, as in the case of a successful course of treatment, the images may no longer be relevant.
Post-acquisition image recall and display may be relevant for comparative purposes, including referrals. The ability to provide access to prior exams may be valuable to assessing the current study, which may or may not be in the same facility or IDN. In such instances, providing convenient and timely access may be valuable in avoiding additional diagnostic exams.
An emerging area of access is patient accessibility. In the past, patient interest in seeing their exam may not have been important. Today, with a proliferation of smart devices, and more technically savvy patients, there is a growing need to image-enable the patient. This is further supported by the “Ditch the Disk” initiative that promotes accessing images from the cloud instead of a physical CD.
The reality is that all these aspects may be drivers for an EIM, but realistically aside from primary imaging areas such as radiology and cardiology, there may not yet be sufficient demand to justify EIM for other drivers.
Typical of implementations is UMASS Memorial Health System in Worcester, MA. According to Scott McAdams, director of ancillary applications and integration, “Radiology and Heart and Vascular are the prime areas addressed by enterprise imaging, while areas such as Pathology have not expressed a desire yet.” UMASS is moving forward to address portable Ultrasound across the enterprise as its next initiative. “We get some requests such as Dental, but since there are no orders associated with the images yet, it is hard to identify the studies,” according to McAdams. Forward thinking, UMASS does have plans to address physician and then patient engagement through interaction between their PACS viewer and their Epic EMR.
Another site that has been working toward an enterprise implementation is UCLA Health System. According to Ilayaraja Elangovan, program manager, Enterprise Imaging, “there is little financial incentive to expand beyond radiology or cardiology as volumes are negligible and difficult to justify the overhead cost although there are other benefits. Enterprise Imaging sounds great, but services don’t appreciate the effort involved to handle the data.” UCLA has had some success in expanding into the Emergency Department and ICUs for portable ultrasound, but they continue to wrestle with physician resistance to placing orders for these exams, according to Ilayaraja.
One of the more advanced enterprise initiatives is that of UW Health in Madison, WI. According to Gary Wendt, M.D., enterprise director of medical imaging, “UW Health started with Radiology, but has expanded beyond that to encompass light images, and has been doing enterprise imaging for fifteen years.” UW Health has been doing electron microscopy imaging since 1997. To address areas that typically do not have an order, Dr. Wendt was instrumental in helping found ImageMoverMD, as chief strategy officer. According to Dr. Wendt, “physicians asked for a method to easily capture images of interest from areas such as dermatology and wound care, and ImageMoverMD provides a convenient means of linking the EMR with PACS for image capture from mobile devices.”
Governance
Another measure of the extent of an EIM is its governance structure. Oftentimes the expansion of imaging follows from an existing service line such as radiology. Leadership very likely is an outgrowth of that service line. Ultimately, Information Technology (IT) will join the effort so as to prevent too many parallel (and costly) individual efforts. In some instances, IT may actually initiate such efforts so as to avoid replication.
Dr. Wendt feels that “governance focus should be on the enterprise.” He also stresses that “images should not live in the EMR, as EMR’s tend to be textual and do not have the rule set’s necessary for images.” Since most initiatives begin with radiology, Dr. Wendt stresses that addressing the enterprise “puts pressure on spending radiology’s budget on other department’s requirements.”
As Ilayaraja explained, “UCLA has run EIM so far as an Information Technology project and is slowly catching up to forming a governance committee. This is in contrast to the way we implemented Epic, where a lot of committees were formed upfront.”
The reality of a true EIM governance is to ensure that most imaging areas are in some way represented, and to assure some degree of impartiality so that no one service line dominates to the detriment of others. A true enterprise governance needs to take all requirements into account so as to not preclude an imaging service from being part of an EIM solution.
Infrastructure
Most imaging environments are a complex collection of multiple systems, EIM being just one of them. Implementing a true EIM will require interoperability with a number of systems, and it cannot be considered standalone.
Two hot topics impacting imaging services include clinical decision support and artificial intelligence. The Protecting Access to Medicare Act of 2014 (PAMA) experienced several delays, but it officially went into effect January 1, 2020 for imaging. PAMA requires physicians ordering advanced imaging exams such as an MRI to consult appropriate use criteria (AUC) through electronic CDS tools, resulting in essentially a pre-authorization-like workflow for Medicare patients.
While the CDS process may be more EMR-intensive on the front end, imaging clinicians will need to be responsible for documenting the consultation with the ordering provider in order to be reimbursed. More than likely this will require a tight integration within the workflow of the imaging service.
Similarly, AI can provide greater efficacy and efficiency to the imaging procedure, impacting the way images are interpreted, as well as the workflow orchestration of how they are accessed. For example, a tight integration between the EMR and EI will enable a more seamless integration of diagnostic information to the diagnostician by providing relevant information from the EMR to the diagnostician at the time of diagnosis.
CDS and AI will ultimately impact more than classical imaging areas like radiology. Requirements would be best served by considering them on an enterprise level, rather than multiple departmental implementations. In UMASS’s case, AI tools are being implemented to enable AI-generated images to be pulled back to the VNA for general availability, according to McAdams. Dr. Wendt feels that AI may be better suited outside of classical imaging such as radiology. “If AI detects something five minutes before a radiologist reviews the case, how do you build a return on investment case? Alternatively, determining a melanoma in Dermatology with AI could impact a timelier appointment. Assessing post-operative images with AI might result in getting the patient on antibiotics easier.”
UCLA has yet to address integration of AI at an enterprise level, as individual departments are doing their own internal developments/deployments, according to Ilayaraja.
While emphasis today is more radiology-intensive, consideration of enterprise applications might have greater clinical and economic benefit.
A realistic approach
EIM can be broadly defined, and it will be up to each organization to determine the definition and strategy they wish to follow. Regardless of scope, every organization should:
- Identify a governance body once a scope has been identified, and secure representation from participating imaging services
- Identify EIM requirements for all imaging services identified, and how best to accommodate them within the identified scope
- Develop a realistic timeframe and budget to address EIM requirements, as it may take several iterations to achieve
- Identify existing infrastructure and how applicable/scalable it is to address the enterprise
- Evaluate ancillary areas such as AI and CDS to determine their role in an EIM strategy
The reality is that imaging has moved beyond the classic boundaries of radiology and cardiology, and organizations need to be thinking about imaging on an enterprise level. Organizations that recognize the need for EIM will experience improved efficacy, quality of care and economies of scale in achieving healthcare delivery improvements.
Joe Marion is a principal in the Waukesha, Wis.-based Healthcare Integration Strategies LLC