Ravi Nemana, MBA, Managing Director Products, Performance Technologies, The Advisory Board Company
Barbara S. Harvath,
RN, BA Public Service/Health, Senior Director, Performance Technologies,
The Advisory Board Company
With the advent of readmission penalties by the Centers for Medicare and Medicaid Services (CMS), clinical and financial incentives are now aligned to promote the reduction of readmission rates. The penalties that created this alignment were the result of CMS’s long-standing efforts to improve quality and learning from a series of demonstration projects that showed[1] that care transition programs improved patient outcomes, including reduced readmission rates. The result: Two-thirds of hospitals faced CMS readmission penalties last year.
In response, hospitals and health systems have scrambled to implement readmission programs to assist in coordinating care and improving patient outcomes. Most hospitals and health systems have instituted care management and care transition programs, but quickly discovered that these programs can be both costly and ineffective without appropriate patient targeting and skillful leveraging of resources, both human and financial. For example, many health systems quickly discovered that while many patients exhibit risk factors for readmission, only a subset had modifiable risk factors that would reduce readmission rates. Regardless of the scale of the program, finding “actionable” patients (i.e., those appropriate for intervention) required chart review and/or assessment, and, as the patient’s state changed, required multiple reviews and tracking of metrics. What health systems needed was a team-based, data-supported approach to care and care transitions analytics.
Analytics, defined here as “finding and showing meaningful patterns in data,” allows organizations to use meaningful metrics to target patients and patient populations, automate patient tracking, streamline workflow and, through the use of text-analytic approaches, even automate chart review. These data-driven approaches help to narrow initiatives to those that benefit the most from care interventions, consolidate information into a shared “story” of the patient and help coordinate care among different clinical disciplines, from social work to nursing to medicine.
Today’s readmissions analytics are embedded in software, fed by the volume of data in a hospital or health system, and data sources can include past data (claims), present (real-time clinical data) or both. In most cases, an EMR is not required for analytics, though an electronic medical record (EMR) can substantially assist data acquisition and dissemination of results. First, risk factors for readmission are gleaned from these data sources. The risk of readmission can then be scored using quantitative, predictive models for readmission. In the case of text analytics, including natural language processing (NLP), readmission risk is qualitatively and/or quantitatively screened, and even extracted, to show the risk factors at play for a particular patient. The most sophisticated models use both approaches to analyze data in real time, gather key insights from physician and nursing notes, score patients, stratify them and justify their score with risk factors garnered from the patient’s record, including those factors found in free-text clinical notes.
Not all risk models are the same, and the best models are often a family of models that work in concert on specific sub-cohorts of patients (aka segmented models). A good quantitative model is compared to what happens in real life and it is characterized by three factors:
- Sensitivity or precision: When the model says there is a risk of readmission, how correct is it?
- Specificity: When the model says there is no risk of readmission, how correct is it?
- Recall: Of those who are actually readmitted, how well does the model predict their readmission?
A last figure, accuracy, predicts the model’s overall ability, but without taking the above measures into account, it can hide the fact that it is much better at finding patients with no risk versus those with readmission risk, or vice versa.
Generally, modelers consider figures of around 80 percent as worthy of implementation, especially when they’ve been tuned to the population being evaluated. Modelers typically suspect models with near 100 percent accuracy as potentially having some methodological flaw or bias, or being tuned to overemphasize one of the above metrics, often specificity. The case for model quality can be further bolstered if models have been characterized by all of the above metrics, funded by government research, published in peer-reviewed literature and/or been vetted by academic or other reputable organizations. This external vetting typically results in the model being run on a large and diverse patient populations, often millions of patient encounters.
We note that all models will have false positives and negatives, where a model will wrongly identify whether a patient is at risk for readmission. The value of high-quality models lies in minimizing this probability and, through improved sensitivity, specificity and accuracy, helps to reduce the resources wasted on inappropriate patients and/or interventions. Given that clinicians cannot sustainably evaluate every chart in the census every day for readmissions, the tradeoff between modeling and human review favors computational models, especially when the models are of high quality.
Analytically driven readmission prevention case studies
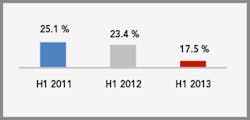
At The Advisory Board Company, we use readmission analytics to help a number of our members achieve meaningful results in tackling readmissions at the scale of their health system. For example, Robert Wood Johnson University Hospital Hamilton used readmission analytics to provide an accurate score to guide inpatient and transition care teams to deliver tiered evidence-based prevention responses. Over a two-year period, they reduced their 30-day readmissions from 25 percent to 17 percent by using a simple but accurate readmission risk score to prioritize their implementation of tiered interventions, align their care teams and contractors (e.g., follow-up calls) to the severity of patient risks and provide consistent and prioritized interventions, with measurement incorporated in their care processes.
Improving quality of care
RWJUHH 30-day readmission rates (Any APR-DRG)
Adding text analytics to predictive modeling improves accuracy and insights to enable better care team decisions. This, in turn, shifts work from case-finding to value-added activities of care coordination. Scripps Health System is using an accurate, real-time predictive readmission score together with text analysis of their free-text EMR data to screen for criteria specific to individual care teams. Using a broad set of computationally detected risk identifiers such as psychosocial issues, non-adherence, disability, complex medication regimens and other factors, care teams identify their patients in near real time, rapidly assess whether intervention is warranted and save substantial chart review time. Scripps care teams can shift their time from case-finding to providing interventions, referrals and testing that specifically targets individual patient deficits, personalizing care to a patient’s individual risks and needs. Analysis of their near 900-patient daily census at their five-hospital system takes roughly 20 minutes and runs multiple times per day, providing just-in-time case information.
In the most intriguing and forward-thinking use of analytics, one of our large Texas members has expanded their use of analytics to cover the continuum of their patients’ experience. Their approach uses analytics to remove the distinction between inpatient and outpatient and applies risk management – clinical, operational and financial – to all patients as appropriate, allowing real-time medical decision-making. Currently, we can process hundreds of thousands of documents per day of varying formats, velocities and document quality – in real time and into one logical “picture” of the patient – to inform care teams across the continuum and prevent patients from “falling through the cracks” during transitions in care. Further, analytics has expanded beyond readmissions to a broader array of analytics that impacts accountable care, patient management, throughput and rapid response to patient adverse events.
Conclusion
Two-thirds of hospitals faced CMS readmission penalties last year. These penalties derived from CMS’ efforts that began more than 20 years ago to improve quality. The advent of readmission penalties by CMS in 2007 has left hospitals seeking scalable solutions. While clinical and financial incentives are now aligned to support reducing readmissions, in the end, analytical support will be crucial to developing a data-driven, scalable approach to care, not only for readmissions, but also for other initiatives such as managing noncompliance, depression, chronic illnesses, palliative care and even operational issues such as length of stay.
1 Promising Models of Care Coordination in Medicare: Lessons for Medicaid Beneficiaries with Chronic Illnesses. 2009. Deborah Peikes, Ph.D., Randall Brown, Ph.D., Greg Peterson, MPA, Jennifer Schore, MSW.