At Houston Methodist Hospital, an initiative to more effectively measure patient acuity in 11 nursing units using electronic health record (EHR) data and predictive analytics has helped reduce the mortality rate in those units by 30 percent, prompting a hospital-wide rollout of the health IT tool to improve care delivery.
Houston Methodist is a 7-hospital health system and the 828-bed Houston Methodist Hospital is its flagship, academic hospital in the Texas Medical Center. According to Houston Methodist St. John Hospital Vice President of Operations and Chief Nursing Officer Katherine Walsh, R.N., the hospital began a project with PeraHealth, a health IT vendor that provides real-time clinical surveillance solutions, back in 2011 as part of a project to conduct a comprehensive retrospective review of patient charts to determine trends in patients’ conditions and whether deteriorating conditions could be predicted. PeraHealth’s clinical surveillance solution is based on the Rothman Index, a disease-agnostic measure of patient acuity that can be used to predict patient readmission and mortality risk. The Rothman Index was developed by Michael Rothman, PhD, a scientist with experience in data analysis and founder of PeraHealth, and his brother Steven, an engineer, following the unexpected death of their mother due to a treatable, yet undiagnosed complication after surgery.
While the mortality rate at Houston Methodist Hospital was already low at the time, with a risk-adjusted mortality rate of 0.70, according to the University Health System Consortium (UHC) risk adjustment model, Walsh says the sudden loss of a patient prompted healthcare leaders to take a second look at health IT tools that could improve patient monitoring and serve as early warning systems.
“When we looked at the patient record and at the Rothman Index, we could see over the course of a couple of days, this patient had been slowly deteriorating. She was in her 30s and she was very ill, so her mortality wasn’t unexpected, but a sudden death was. When we looked at the data and the Rothman Index score, we saw that she had been deteriorating subtly for days but it wasn’t outwardly apparent because she had been very ill. That was a wake-up call to some of us,” Walsh says.
Hospitalized patients frequently exhibit subtle warning signs in the hours and days before experiencing life-threatening health problems. And while physicians and nurses at Houston Methodist Hospital are highly skilled to detect this deterioration, the sooner the detection, the more likely the care team can intervene successfully. And, a five-day hospital stay typically includes an average of 25 patient handoffs, so subtle warning signs may be missed during handoffs, department transfers and special procedures.
Katherine Walsh, R.N.
Health system leadership recognized an opportunity to improve care delivery by enabling physicians and nurses to better monitor patients for subtle but serious health issues. Beginning in 2013, Houston Methodist began implementing PeraHealth’s clinical surveillance solution for acute care in 11 nursing units, including medical units, surgical units, oncology, orthopedics and a gynecology unit.
“Rather than try to retool the nursing care delivery model and get our doctors involved, we took a few steps back and said let’s simplify this and let’s pick a couple of units, train the staff and get them involved in it and treat it as a nursing-driven tool,” Walsh says.
She continues, “We implemented this in a cross section of different units as well as units that I knew the leaders were open to change and were enthusiastic and energetic. I was trying to create change where I knew I had folks that would be amenable to making this happen.”
In conjunction with the PeraTrend software rollout at Houston Methodist Hospital, a training agenda also was deployed, including grand rounds presentations, classroom training and hands-on use of the program. The program also had three designated champions—a project manager, a nurse educator and a clinical nurse specialist—who worked with Walsh to oversee the training and implementation.
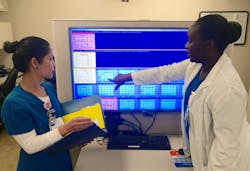
The clinical surveillance software pulls data from the EHR system and the data is automatically translated into a Rothman Index score that’s presented in color-coded graphs, enabling care teams to quickly visualize patient condition. Overlaid on the Rothman Index data is a set of hospital-customized rules, designed to highlight graphs for patients who have either fallen to a low Rothman Index score or have experienced a significant drop in score over a given period. Graphs can be viewed in the EHR or displayed side-by-side on interactive monitors, allowing clinicians to view updated conditions for multiple patients at a time. The patients can be risk-stratified on the screen with highest risk at the top, then high risk, followed by moderate risk. Patient acuity is calculated each time a new element is entered and translated into a Rothman Index score that’s presented in color-coded graphs trending patient condition, with red representing highest risk, followed by yellow then blue.
Along with vital signs and lab results from the EHR, the clinical surveillance solution implemented at Houston Methodist also incorporates nursing assessments which is a unique data point that can help identify signs of deterioration, Walsh says. And, she adds that the clinical surveillance solution does not require any manual data entry for staff and was easily integrated into clinicians’ workflow.
“The beauty of this is that it doesn’t require you to do anything new. There a lot of things that come out in healthcare that are supposed to make jobs easier, but for the people at the bedside it actually makes it harder. This takes the variables that you are documenting anyway and arranges them in a way that makes sense."
She continiues, "If someone sat at a chart and tried to put this together, the amount of time to do it, and knowing where and what to pay attention to, doing that manually would be too unwieldy in terms of being able to do that as a part of patient care,” she says.
In addition to training, protocols were established requiring nurses to reassess patients if an alert was triggered. Nurses also frequently monitor patient status by referring to the dedicated monitors at nursing stations. As the program was implemented, clinicians experienced first-hand how the clinical survelliance tool aids with detecting early signs of deterioration.
“If our neuro-ICU unit called and said they were sending us a patient, then I would pull up the Rothman Index and if the score was not completely stable, then I’d say, 'No, you’re not sending this patient home, let’s stabilize the patient first.' So that was a save,” Walsh says. “And, during clinical care rounds, nurses would check the Rothman Index. If they identified that a patient was deteriorating they would then call in a doctor or an emergency response team and there were able to turn the patient’s condition around rather than just send them to the ICU. That was a save. As we got these saves, we started talking about them and the stories kept the momentum of the program going.”
The program’s initial results indicated a decrease in mortality rates; yet some healthcare leaders were skeptical about the cause of the fall in the mortality rate. Walsh and her team then conducted an 18-month analysis, from January 2014 to June 2015, of 33,797 patient encounters, including nine months of prospective data review after the implementation of the clinical surveillance tool.
The analysis found that the mortality rate in the 11 nursing units utilizing the tool fell 30 percent and the risk-adjusted mortality rate fell 32 percent to 0.49. And, the sepsis mortality index was 8 percent lower compared to non-study units.
Walsh refers to the clinical surveillance solution as a “safety net” that gives the nursing team another set of eyes.
“It gives us a tool that makes our jobs easier and gives us an ability to identify, more quickly, things that we would have identified but perhaps not as readily,” Walsh says. “When it comes to monitoring patients for signs of deterioration, there is a normalization of variance over time. This enables us to look at a patient’s condition over a span of time. It might be normal for a patient to breathe eight times a minute, but not if that patient had been breathing 16 times a minute eight hours earlier, so that tells you that something is different.”
Following the results of the analysis, Houston Methodist Hospital continued to roll out the software to other nursing units, and by this past November all the hospital’s nursing units have implemented it. This spring, the Houston Methodist health system plans to implement the clinical surveillance tool in its other six hospitals.
Michael Rothman, PhD
Michael and Steven Rothman were inspired to develop the Rothman Index as a patient acuity measure after the avoidable death of their mother in 2005 from a common complication after a low-risk surgical procedure.
"My brother and I felt that the doctors and nurses at the hosopital were competent, but it seemed that the system itself failed. The doctor could come in and evaluate my mother and say, 'That’s a reasonable condition for someone so many days after a surgery,' but what he couldn’t do was see the trend. Each day she was seen by a different doctor or nurse and nobody could connect the dots. We asked, 'Why isn’t there a simple score that indicates a patient's condition and that you could plot over time and see if someone is getting sicker or better?"
The Rothman Index has been validated by 18 peer-reviewed publications and is now in use in 80 hospitals and clinics as part of PeraHealth’s clinical surveillance solutions. Walsh credits Michael Rothman’s work in data analysis, rather than healthcare, as an advantage in the development of the clinical measure to predict patient readmission and mortality risk.
“Those of us in healthcare come with a set of biases and he didn’t have that bias. He kept asking questions about the nursing assessments and about the changes in patient conditions and then he put the science behind it and it offers a fresh perspective,” she says.