Kathleen C. Aller, InterSystems
Preventable readmissions are estimated to add $25 billion to the cost of U.S. healthcare annually, representing about 11 percent of all insured patients. Public and private payers have made it a priority to reduce this rate and have implemented a number of incentive and penalty programs to encourage providers to address the issue locally. Intervention programs around the country have shown encouraging results, usually through a combination of identifying at-risk patients, redesigning discharge processes and coordinating follow-up care across the community.
Many readmission reduction programs are “high touch” and involve a broad network of providers and services, which makes them difficult to scale and maintain without information technology to assist. Among the patients at highest risk for readmission are those with multiple chronic conditions who may see upward of a dozen providers for their care. An information management, or analytics, platform that can effectively integrate this network, measure progress against the care plan and intervene in a timely fashion as needed can mean the difference between small, short-term reductions in preventable readmissions and significant, sustainable change.
Closed-loop systems
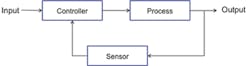
Virtually all readmission reduction programs can be characterized as closed-loop feedback systems (Figure 1), a concept derived from electrical engineering. Closed-loop systems like thermostats, clothes dryers or ovens rely on sensors such as thermometers to measure actual conditions, compare them to a goal such as cooking temperature and adjust the process (e.g., heating) to keep it on track.
Figure 1: Simple closed-loop system.
Well-designed closed-loop systems reduce errors by identifying points of failure, recognizing deviations from what is expected and automatically adjusting processes. This process produces stability and enables reliable, repeatable and cost-effective performance. For this reason, closed-loop systems have been widely adopted as business models. In healthcare, for example, they are used to describe clinical and administrative processes such as medication ordering and administration or referral management.
Readmission reduction as a closed-loop system
Complex healthcare processes require multiple feedback loops and failure detection mechanisms, but can be simplified to their most basic elements for purposes of illustration. For readmission reduction, the process is managing a population of patients following an inpatient stay. In essence, the desired output is a patient who has returned to a healthier status after hospitalization. If the system works well, the patient receives proper follow-up care from his or her care team, until he or she is on a path back to health. If there is a system failure, and the follow-up care does not occur, the patient may end up being readmitted (Figure 2).
At a population level, we want to know whether the rate of readmissions is moving down (desired state) and, if not, we want to intervene automatically to move the trend in the right direction.
Analytics redefined
The term analytics has come to be associated with visual dashboards, yet these are only one aspect of a robust analytics platform. A closed-loop model for readmission reduction begs the question, “Am I making steady, incremental progress toward my goal?” If not, it initiates corrective action. This requires information technology capabilities to integrate comprehensive data, reason over that data to measure progress, intervene in a timely fashion and support continuous process optimization. Looking at these capabilities further, closed-loop readmission reduction systems:
- Bring together information from across the care process. A clothes dryer needs information about airflow, moisture level and temperature to manage the drying process. Readmission reduction systems need comprehensive, relevant information from all components of the care system, including clinical systems, financial systems and information supplied directly by the patient. For example, if we are targeting readmission reduction for congestive heart failure, relevant data might include not just traditional claims, but pending test results available post discharge and patient-entered data related to self-care. On the other hand, we can’t wait to have every data element we might ever need. We need a flexible analytics data store that eliminates data silos and can grow in breadth and depth as new data needs are identified.
- Are able to measure progress by reasoning over heterogeneous data. Measurement implies knowing the baseline and the desired endpoint, or trend direction. It also implies being able to understand both structured and unstructured data. Too often, we rely on proxy measures, or our systems are inadequate because they address only one aspect of the problem. We need analytics systems that can use the heterogeneous healthcare data in our analytics data store to measure care for both individual patient records and entire populations.
- Rely on incremental change and continually compare performance to the goal. An oven that measures the temperature once an hour produces burned cookies or soggy soufflés; it needs to assess performance more frequently. Data capture and measurement must always be appropriate to the intervention timeline for a feedback system. Furthermore, it must support each of the relevant incremental data points. For readmissions, this implies that our analytics can quickly and automatically identify a dynamic target population, initiate post-discharge care coordination during hospitalization and enable appropriate measurement and intervention across the entire care team throughout convalescence, and in particular during care transitions.
- Apply active interventions to keep the system moving in the right direction. Your thermostat automatically takes corrective action each time it senses the temperature is out of range. It may also alert you to points of failure in the system such as a clogged air filter. Similarly, analytics for readmission reduction must be able to intervene in ways that are both timely and appropriate. Score cards and reports support long-term trend analysis, but are inadequate for real-time patient care. Care providers need to be notified proactively to rectify gaps in care, avert potential errors or address poor process coordination. This may mean having your analytics system reach directly into any number of EHRs or other applications such as care management systems. It may mean sending a text or email to one or more team members. It might even mean generating a phone call directly to the patient.
An analytics platform that includes these capabilities can sit at the core of a closed-loop process and be continually adapted to address new populations of interest.
Finally, if we look at newer consumer electronics such as the Nest thermostat, we see these are actually learning systems, applying the data they capture from past events to optimize future performance. Similarly, our readmission management analytics capabilities need to support a learning health system, reusing the data captured as a byproduct of care to identify what works, what does not and where the next best opportunity for improvement may lie.
Real-world analytics-enabled readmission reduction
The Rhode Island Quality Institute (RIQI) operates CurrentCare, the health information exchange for the state of Rhode Island. One of the great strengths of that exchange is the way in which the RIQI has used it to create a learning health system. Data that is captured for care is used for continuous system improvements, including reducing readmission rates.
Figure 2: Simple readmission management closed loop.
Many readmissions are due to lack of coordinated follow-up care after discharge. Physicians told the RIQI that they often have no knowledge that their patients have been hospitalized until too long after the fact. So the team created Hospital Alerts, a simple closed-loop feedback process to test the hypothesis that timely information about hospital care would lead to better follow-up and reduce readmission rates. Hospital Alerts is a service where primary care providers can be automatically notified of a hospital or emergency department admission or discharge; it also allows non-primary care providers to subscribe to notifications about their patients. When a patient is admitted or discharged from a RI hospital or emergency department, an alert is generated to the appropriate provider.
- The analytics for the Rhode Island readmission example demonstrate all of our identified requirements:
They capture and measure appropriate data; - Alerts are automated, appropriate and delivered immediately to the care provider along with access to relevant clinical data; and
- Potential care gaps are identified in a timely fashion and care management actions taken based on the alert and the accompanying clinical data.
The data captured during the process of care supports continuous improvement.
Initial results in Rhode Island are promising: a 15.7 percent reduction in the overall admission rate for those CurrentCare patients whose providers received Hospital Alerts versus CurrentCare patients whose providers do not receive Hospital Alerts. With full adoption, this represents potential annual savings of $25.8 million across the entire state.
Summing up
The RIQI example illustrates a closed-loop feedback system at its simplest, yet it achieves impressive results. Closed-loop processes intended to address readmission reduction for specific patient subpopulations typically need multiple feedback loops and may need to intervene at many points in the care process. A comprehensive analytics platform designed to look across the continuum and automate interventions to the entire care team can make such complex readmission reduction programs scalable, sustainable and adaptable.