“The surest path to robust interoperability is to enable market forces to drive us forward.”
Hype
- n. extravagant or intensive publicity or promotion.
- v. to promote or publicize (a product or idea) intensively, often exaggerating its importance or benefits.
FHIR and the Hype Cycle
Have you noticed the hype around Fast Healthcare Interoperability Resources (FHIR)? It was hard to miss at HIMSS2018, where enthusiasts proclaimed that FHIR will solve our interoperability woes. It will not, and it is essential we dispel the misconceptions and hype—for they pose significant risks to fixing our broken healthcare system.
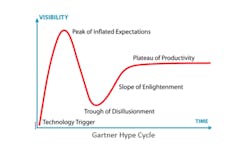
Hype often accompanies the emergence of new technology. The Gartner Hype Cycle, a well-known guide to healthcare technology life-cycles, can be fascinating and useful in understanding these natural occurrences.
The hype cycle reminds us that while enthusiasm, optimism and high expectations are commendable, reality tends to have a way of humbling our best intended efforts. As a CMIO and healthcare consultant, I have watched this play out countless times. We are all subject to falling for hype and I confess that, at times, I have been either a perpetrator, a victim or both! Being aware of this cycle is a good way to guard against the ill effects of buying into the hype.
It’s important to be clear about two things. First, the folks actually working to develop FHIR are consistently the most realistic and cautious in making claims. They bear little, if any responsibility for the surrounding hype. Second, while FHIR has limitations just like any technology, there’s nothing wrong with it per se. Quite the opposite. I favor almost anything that moves healthcare away from using outdated legacy integration technologies and towards the API-based approach that enables interoperability in the rest of the (non-health care) digital economy.
FHIR is not the problem. The problem is the misconceptions and hype surrounding FHIR. It’s vital we address those misconceptions and mitigate the risks posed by the hype.
Four Hard Truths About FHIR
There is a common misbelief that FHIR is going to provide a rapid path to robust interoperability between third-party applications and electronic health records (EHRs). Many believe FHIR will result in a standardized plug-and-play approach for rich data exchange. Just plug your application into FHIR and you are off and running!
This is flat out wrong for at least four reasons:
- FHIR is not a standard, it is a “suggestion”. The biggest FHIR misconception is that it will be an industry standard. In theory, FHIR could be a standard. In practice, there are no enforcement mechanisms and EHR vendors (and others) have already implemented different versions of FHIR. It is clear that FHIR is NOT going to be a robust standard that is consistent across implementations.
- EHR vendors are not implementing all available FHIR APIs. This creates another critical source of inconsistency. Developers who rely on FHIR for EHR integration must keep track of which EHRs have implemented which APIs. A robust API provided by one EHR may be completely absent in another.
- EHR vendors are not consistently implementing the entire API. Even if two vendors implement the same FHIR API, they may not implement the entire specification for that particular API. One may have all data elements, while the next only includes a portion of the specification.
- FHIR extensions undermine standardization. In principle, allowing developers to extend upon the basic FHIR specification can have advantages. In practice, this further undermines any attempt to create a standard. History shows that permissive models—like “z-segment” customization of HL7—opens the door to the wild west and results in divergence rather than convergence.
These are not theoretical concerns. FHIR endpoints are being implemented differently by EHR vendors. This is clearly illustrated in Table 1 below (and in a more detailed analysis here).
This reality places huge limitations on FHIR and largely defeats the purpose of having a standard specification in the first place. We have seen this movie before and it does not end well! Both HL7 and CCD have had well defined specifications but did not control the implementation. Sorting out the many different flavors and maintaining fragile, one-off implementations is a nightmare and a huge waste of resources for application developers and integration teams. It is also an enormous barrier to innovation. Unfortunately, FHIR will not solve these problems and may make things worse by introducing even more variants.
Why the Hype Matters
Lack of robust interoperability is the most important issue in healthcare IT today. Widespread deployment of EHR silos that don’t interoperate with each other and inhibit the wider exchange of data has cast a harsh light on these problems. When health system leaders and digital health innovators consistently cite lack of interoperability as one of their biggest challenges, you know it’s a big deal. The recent announcement by CMS that they will be retooling the meaningful use program to place more emphasis on interoperability provides further confirmation.
The stakes are exceedingly high. Health systems are dealing with enormous economic pressure, increasing competition and market turbulence. They recognize they must innovate and leverage healthcare IT (HIT) to enable greater value and satisfaction for patients and providers. The same applies to digital health companies. In short, lack of robust interoperability is the biggest bottleneck in healthcare innovation and must be rapidly resolved.
Which brings us to the risk associated with FHIR hype. Too many are placing too much faith in one unproven approach. Putting all our interoperability “eggs” in the FHIR “basket” is a single-threaded approach that greatly compounds the risk of failure.
Instead, we should mitigate the risks by pursuing diverse solutions. Just like you shouldn’t bet your retirement on a single stock, we shouldn’t be betting on a single approach to solve a complex issue like interoperability. Healthcare needs a mix of legacy technology, FHIR APIs, EHR vendor APIs and commercial APIs. This diversity allows us to match the best solution to the problem at hand, lessens the risk of relying on any one solution and promotes competition.
This last point is vital. The surest path to robust interoperability is to enable market forces to drive us forward. This will rapidly produce a variety of options, as competitors race to provide the best performance at the lowest price.
Dr. Dave Levin has been a physician executive and entrepreneur for more than 30 years. He is a former Chief Medical Information Officer for the Cleveland Clinic and serves in a variety of leadership and advisory roles for healthcare IT companies, health systems and investors. You can follow him @DaveLevinMD or email [email protected].