The Centers for Medicare & Medicaid Services (CMS) is proposing major policy changes to the Medicare Physician Fee Schedule and Quality Payment Program, with the overarching goal to further reduce clinician burden.
At the core of the proposed policy changes, the agency announced on July 29, is a desire to improve the Quality Payment Program (QPP) under MACRA (the Medicare Access and CHIP Reauthorization Act of 2015) by streamlining the program’s requirements. The proposal calls for a simpler way for clinicians to participate in CMS’ pay-for-performance program, the Merit-based Incentive Payment System (MIPS), which is one of two payment tracks within the QPP.
This new framework, called the MIPS Value Pathways (MVPs), beginning in the 2021 performance period, would move MIPS from its current state, which requires clinicians to report on many measures across the multiple performance categories, such as Quality, Cost, Promoting Interoperability and Improvement Activities, to a system in which clinicians will report much less, CMS officials contend.
Under MVPs, clinicians would report on a smaller set of measures that are specialty-specific, outcome-based, and more closely aligned to Alternative Payment Models (APMs). MVPs will connect activities and measures from the four existing MIPS performance categories that are relevant to the population they are caring for a specialty or medical condition, according to CMS.
Per the proposal, “MVPs would utilize sets of measures and activities that incorporate a foundation of promoting interoperability and administrative claims-based population health measures and layered with specialty/condition specific clinical quality measures to create both more uniformity and simplicity in measure reporting. The MVP framework will also connect quality, cost, and improvement activities performance categories to drive toward value; integrate the voice of patients; and reduce clinician barriers to movement into Advanced APMs.”
The QPP, which started on Jan. 1, 2017 with a “pick-your-pace” program year—which essentially enabled clinicians to avoid payment penalties as long as they submitted at least the minimum amount of quality data—has since ramped up the requirements for participating clinicians. At the same time, CMS continues to exempt certain clinicians who don’t meet a low-volume Medicare threshold. There doesn’t appear to be any changes to the low-volume threshold for 2020 in the new proposal.
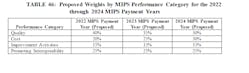
The proposed rule also suggests changes to how the four performance categories will be weighted for performance years 2020 through 2022 (payment years 2022 through 2024), which can be seen in the table below from the proposed document.
CMS is still looking for stakeholder feedback regarding the structure and focus of the MVPs, as well as what other criteria the agency should use to select measures and activities.
In all, the proposals to the PFS, QPP, and other Medicare Part B payment policies for calendar year 2020 make up a 1,704-page document.
Billing and Coding Changes
For 2019, CMS finalized changes to simplify billing and coding requirements for certain office-based visits known as evaluation and management (E/M) services, responding to longstanding criticism that they were burdensome and overly complicated. Those changes, the first to the E/M framework in more than 20 years, aimed to give clinicians new flexibility to consider time with the patient or medical decision-making in how they code an E/M visit, so they could focus more closely on what is clinically relevant and medically necessary for the patient. For instance, the agency finalized single blended payment rates for both new and established patients for office/outpatient E/M level 2 through 4 visits, in turn collapsing the number of codes to make it easier on clinicians.
The proposed changes for 2020 would build on these policies by paying clinicians across all specialties for the time they spend treating the growing number of patients with greater needs and multiple medical conditions, through increasing the value of E/M codes for office/outpatient visits and providing enhanced payments for certain types of visits, CMS said in a press release. “This is especially important to certain specialists that spend significant time managing patients with multiple co-morbidities, such as diabetes and heart disease,” the agency stated.
CMS is also proposing to take steps to help clinicians better manage chronically ill patients, particularly during their transition from hospital to home. The proposed rule would increase payments to practitioners for time spent on care management after a patient leaves the hospital ensuring proper follow-up and continuity of care for patients.
And, for the first time, CMS is proposing to pay for care management services for patients with a single, high-risk chronic condition such as diabetes or high blood pressure. CMS is also proposing to pay clinicians more for additional time spent on care management activities for patients suffering from multiple chronic conditions.
The proposed rule also calls for expanded Medicare coverage to pay opioid treatment programs (OTPs) for delivering Medication-Assisted Treatment (MAT) to people with Medicare suffering from opioid use disorder (OUD). Opioid Treatment Programs (OTPs) are programs or providers that provide a range of services to people with opioid use disorder, including medication-assisted treatment and counseling. OTPs must be accredited by the Substance Abuse and Mental Health Services Administration (SAMHSA), and CMS is also proposing to make a new monthly bundled payment to practitioners for management and counseling involving MAT for patients with opioid use disorder.
This proposed rule is projected to save 2.3 million hours per year in burden reduction, according to CMS. “Clinicians are drowning in paperwork and reporting requirements caused by cumbersome government rules and regulations,” said CMS Administrator Seema Verma. “These administrative costs add to the total cost of delivering healthcare, which means physicians often have to hire extra staff and spend more time complying with requirements instead of with their patients.”
One stakeholder group—the Virginia-based AMGA---has already lashed out against the proposal, remarking in a statement that the “estimated program year payment adjustments for 2020 MIPS do not reflect congressional intent or provide reimbursement that is commensurate with the investments that AMGA members made in response to MACRA.”
The AMGA statement took issue that per the MACRA law, providers have the opportunity to earn an adjustment of up to 9 percent on their Medicare Part B payments in 2022 based on their 2020 performance. “However, as indicated in today’s proposal, CMS estimates the overall payment adjustment will be 1.4 percent,” the group said. As such, “AMGA is concerned that MIPS is no longer a transition tool to value-based care, but instead represents a regulatory burden that does not support physician group practices and integrated systems of care that are investing in delivery models based on care coordination and improving population health.”
“We are entering the fourth year of MIPS, and our members expected to have the opportunity to earn a significant payment adjustment if they performed well,” said Jerry Penso, M.D., AMGA president and CEO. “By proposing an overly cautious approach, CMS is not rewarding those organizations that made the necessary investments in and championed value-based care as envisioned by congressional leaders.”
Public comments on the proposed rules are due by September 27, 2019.