Leaders at the Framingham, Mass.-based Definitive Healthcare on Oct. 20 released the results of a study that they’ve produced, based on medical claims data, that provides a different lens through which to look at clinician staff shortages in hospitals, medical groups, and health systems.
The report, “Addressing the Healthcare Staffing Shortage,” involved an analysis of data from Definitive Healthcare’s ClaimsMx and PhysicianView products, with the analysis focusing on the numbers of providers billing each year, by primary specialty on medical claims, based on August 2022 data. The report was written by Ethan Popowitz, with contributions by Todd Bellemare, senior vice president of strategic solutions, and Maggy Tieche, market research manager, at Definitive Healthcare.
Key findings include:
> 333,942 healthcare providers dropped out of the workforce in 2021
> 33 percent of all physicians are over 59 years old. The average age of a nurse is 57, psychiatrist is 55, surgeon is 56, and family practice physician is 52
> Internal medicine was the specialty that lost the most providers in the last year, followed by family practice and emergency medicine
> The largest healthcare systems added 10,000 beds, 35 hospitals, and 163 physician groups in the past three years
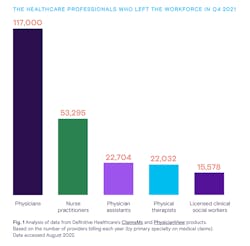
Based on their analysis, the Definitive Healthcare leaders believe found that 117,000 physicians left the workforce in the fourth quarter of 2021, while 53,295 nurses did so (see figure 1). It was not possible to extrapolate departures of nurses who do not submit claims, since the statistics analyzed were those of claims submissions.
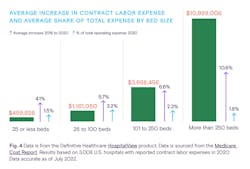
The analysis also found that the average increase in contract labor expense rose dramatically as a percentage of total organizational expense by bed size, with a 4.1-percent increase for contracted labor being far more devastating to hospitals with 25 or fewer beds, than a 10.6-percent increase for hospitals with more than 250 beds (figure 2).
Healthcare Innovation Editor-in-Chief spoke with Todd Bellemare about the study’s results, and their implications for the healthcare industry. Below are excerpts from that interview.
What do the results look like to you, overall?
To be honest, somewhat scary. People have been talking about the physician shortage; for the pandemic to exacerbate that, is even more frightening. At the top of the 2010s, people predicted there would be a physician shortage. And looking at that exacerbation of losing physicians, especially in the PCP space, we saw a lot of internal medicine physicians—as well as nurse practitioners—falling away. The feeling was that, yes, some PCPs might fall away, but we’d have NPs and Pas. But looking at everything across physicians and non-physicians; and with 300,000 folks dropping out of the workforce during that two-plus-year timeframe in 2020 and 2021, is really scary. The first chart [figure 1 below] looks at Q4 of 2019 as a baseline, and then compares it to Q4 of 2021. And whenever you’re looking at a medical claims database, you have to look at consistent panels of billing providers. And when we looked at the timeframe, going back to 2019 for a baseline, we looked through 2021.
And 2020 through 2021, who did we lose? We’re talking about both allied health professionals and physicians. Page 4: we actually lost 117,000 physicians from 2019 through 2021. And that doesn’t mean they won’t come back. 117,000 physicians out of 230,609. And nurses do not show up in medical claims data sets; you can only get the nursing data from surveys.
Hospitals remain largely in crisis with regard to traveling/agency nurses. What are your thoughts about that situation? I understand that your analysis was based on claims, so that nurses who submitting medical claims wouldn’t appear.
It’s really an outcropping of people leaving the workforce. So if you lose 10 percent of your NPs or whatever percentage of your nurses, you’ll be looking at a percentage of your workforce; and the prices, as we saw in the data, for contracted nurses, exploded. And we are seeing a bit of a catch-up; but you can only go so long with such difficult margins. Every hospital, when they’re doing their elective surgeries—a good year will buoy them for a number of years; but the reverse is true as well. And there were hospitals and health systems that had to let some physicians go, even though they needed them, because of the cost. And a lot of the supply chains are just starting to get fixed. Hospitals and health systems are still in a deficit situation and are trying to make up for income lost during the height of the pandemic, and if labor costs continue to be high, they’ll still struggle with their bottom lines.
All of this hits rural providers very hard, correct?
Yes. One of the more interesting things; and it’s not new, but urban facilities typically have more money. So when the time came for them to recruit people as they began to bounce back financially a bit, they were able to pay higher salaries. [figure 2]. And the gap between what urban and rural facilities can pay, is astronomical. And we’re already short on PCPs and on nurses. And it’s a domino effect of facilities no longer particular services; OB/gyn services, substance abuse care services, are closing down. Perhaps we can bring down barriers in terms of the cost of medical school; perhaps that might make some difference.
How will the aging of the population and the explosion in chronic illness impact all of this?
The first thing that comes to mind is home health. The need for home health aides is skyrocketing. And if we were able to achieve greater cross-collaboration among states around licensure, to make it easier for folks to move across state lines, especially for home health, that would help. Your comment on Japan made me think about this: some robotic advances might help.
What would your core advice be to the members of hospital and health system c-suites?
It’s almost HR 101. Your “keepage” is so important—keeping your clinicians. The less administrative work you give to physicians, the happier they’ll be. And of course, salary is important. So one of the suggestions I’ve heard is bringing on a Chief Talent Officer, who is involved in getting the right people in the door and hugging those people close, keeping them as happy as you can, including through making sure they’re doing as little administrative work as possible. And the flip side of that is… The amount of medical literature coming out every week is overwhelming; so, helping physicians with the incoming waves of information, whether it be ordering programs, or physician assistance. Those are some of the main things for the c-suite to keep in mind.