Colorectal cancer is a devastating disease. As of 2019, it was the second leading cause of cancer death among all U.S. adults. This year, the US Preventive Services Task Force (USPSTF) is expected to adopt new recommendations for colorectal cancer (CRC) screening which will lower the age of screening from 50 to 45, due in part to the alarming rise in CRC incidence among people under age 50 (up 51% since 1994).
While the data supports lowering the age for screening, it also creates an unfortunate log jam for our medical groups and health systems.
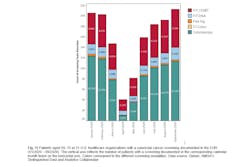
Our national goal for screening patients is 80%, but current data shows that we are behind the national average by more than 10%. Furthermore, data from AMGA’s Collaborative for Performance Excellence shows a significant decrease in the overall volume for CRC screening due to the impact of COVID-19 on practice operations.
Medical groups and health systems will be tasked with closing the gaps created by COVID-19 by screening more patients for CRC. Yet, many of these organizations don’t have enough specialty providers on hand to perform the number of colonoscopies necessary to close that gap. The Mercy Health System, headquartered in St. Louis, recognized that in order to screen all eligible patients for CRC, each one of their gastrointestinal physicians would need to perform eight to nine colonoscopies per day for 230 consecutive days, and they would still need to hire an additional 67 physicians!
“COVID-19 is going to be around for a while—this is our new reality—so we as healthcare organizations have to figure out a way to keep quality moving forward, thinking outside the box," said Elizabeth Keane, chief of population health, SIMEDHealth (Southeastern Integrated Medical), a multispecialty physician group based in Florida.
As we begin to emerge from COVID-19 and get back to “life as usual,” it will be particularly challenging to motivate a 45-year-old patient who has been in quarantine for over a year to take more time out of their life for a colonoscopy prep, procedure, and recovery.
Fortunately, alternative screening tools are available for CRC screening, and they are recommended as equivalent to colonoscopies by the USPSTF. Non-invasive stool-based screening methods, such as fecal immunochemical tests (FIT) and multi-target stool DNA, are practical options that can be completed at patients’ home, and solve numerous access and care gap issues. Furthermore, while social distancing restrictions and patient hesitancy are still significant challenges, the at-home, stool-based screening methods present an ideal opportunity to get more patients screened.
“We really think it’s important now to lead with the FIT, as all of the modalities are equal in their ability to screen and follow up with a colonoscopy,” said James Rogers, M.D., vice president, adult primary care, Mercy Clinic Springfield Communities, based in Missouri.
Data supports that, given the option, more patients will be screened, with many opting for the non-invasive screening methods over the proverbial “gold standard,” traditional methods. A study done at the University of Washington School of Medicine showed that patients who were recommended a colonoscopy were less likely to follow through with screening (38%) than those who were recommended a non-invasive option (67%), or given a choice between a non-invasive option or colonoscopy (69%).
Now is a great time to initiate a conversation with your provider teams about incorporating non-invasive testing options in your practice. There are numerous helpful resources available on AMGA’s website, including white papers and best practice documents, that can help reinforce the viability of these non-invasive testing options in real-world practice settings. At the end of the day, non-invasive testing methods can help close care gaps, reduce total cost of care, and save patient lives. As the saying goes, the best cancer screening test is the one that gets done.
John W. Kennedy, M.D., is the president of the AMGA Foundation and chief medical officer of AMGA. Dr. Kennedy previously served as division director of endocrinology at Geisinger Health System in Danville, PA, where he led the clinical, education, research, and quality program development and expansion for the health system.