Is remote patient monitoring, which has been welcomed by many in healthcare as supporting improved care management of patients with chronic illnesses, now being overused? The subject is a complex one, with nuances. Now, a team of healthcare policy researchers has addressed the issue, in an article entitled “Remote Patient Monitoring—Overdue or Overused?” in a Perspective article published in The New England Journal of Medicine online on April 15.
The article’s authors—Keizra Mecklai, Nicholas Smith, Ariel d. Stern, Ph.D., and Daniel B. Kramer, M.D., M.P.H., are from Harvard Medical School (K.M., N.S., D.B.K.), Harvard Business School (K.M., N.S., A.D.S.), the Harvard–MIT Center for Regulatory Science (A.D.S.), and the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology, Beth Israel Deaconess Medical Center (D.B.K.) — all in Boston; and the Health Innovation Hub, German Federal Ministry of Health, Berlin (A.D.S.), respectively.
Mecklai et al write that “The Covid-19 pandemic has challenged clinicians to find innovative ways to provide essential services while minimizing risks for themselves and their patients. These approaches increasingly leverage remote patient monitoring (RPM), using technology to support treatment for chronic conditions. As the use of RPM services grows, clinicians, payers, and patients face important questions regarding the volume, value, and appropriate use of this care model.”
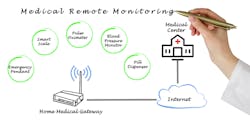
Further, they note that “RPM has long been integrated into focused areas of disease management, such as care of patients with pacemakers or implantable cardioverter–defibrillators. RPM for these patients can reduce costs and supplement or replace in-office care, while offering convenience and heightened surveillance for clinical events. In recent years, RPM technology has expanded into new areas, including chronic and acute care management for multiple common conditions. Devices used in patients’ homes now capture physiological parameters such as weight, blood pressure, oxygen saturation, and blood glucose levels and transmit these data to clinicians for review. For example, wrist-worn pulse oximeters transmitting oxygen-saturation data may be used to monitor lung function in patients with chronic obstructive pulmonary disease, and continuous glucose monitors may wirelessly transmit to physicians information about blood-sugar control in diabetic patients at different times of day and between office visits.”
The article’s authors cite three issues in particular. First, there is the fact that there are no established standards for the demonstration of clinical effectiveness in disease management, for remote patient monitoring technology; indeed, as the researchers note, “A pulse oximetry system for patients with chronic lung disease, for example, may have to meet certain engineering and manufacturing standards but does not need to be shown to improve patient outcomes to be legally marketed. For these devices in general, the Food and Drug Administration (FDA) places the burden on health care providers to ‘develop appropriate processes and procedures to assess and manage risks associated with the integration of [radiofrequency] wireless technology into medical systems.’” Second, as they note, “[T]o date CMS has offered few stipulations on what specifications or standards must be met for coverage of an RPM device. Even well-studied devices in common diseases, such as hypertension, heart failure, and atrial fibrillation, have shown highly variable benefits of different products and care pathways.” In fact, they note, “Randomized, controlled trials have revealed variable effects on outcome measures such as hospital readmission, cardiovascular mortality, or all-cause mortality. Eventually, high-quality, prospective studies either designed as clinical trials or leveraging real-world data will be necessary to support the clinical case for RPM systems.”
Third, “[E]ven without high-quality clinical data, expansion of fee-for-service reimbursement for RPM services provides incentives for rapid uptake. With more and more devices available, providers may enroll large numbers of patients in RPM programs with little regard for who will see a meaningful benefit. Alternative payment models such as bundled payments may shift these incentives, but fee-for-service reimbursement remains a dominant feature of U.S. health care. The costs of RPM expansion may also be borne partially by patients. RPM could increase out-of-pocket expenditures, depending on coinsurance and access to devices, since one established RPM Current Procedural Terminology (CPT) code allows providers to bill for up to 30 minutes per patient per month without having to communicate with the patient or caregiver.”
Meanwhile, the authors have developed a data model “integrating the number of beneficiaries, chronic conditions per beneficiary, utilization of RPM, and reimbursement per RPM service,” to predict the overall cost to CMS of RPM enrollment limited to patients with multiple chronic conditions: even in that subpopulation alone, they write, such enrollment “could translate into annual expenditures exceeding $18 billion, even with just 50-percent uptake,” based on the assumption that 68 percent of Medicare fee-for-service beneficiaries—about 25.4 million patients as of September 2020, would qualify. As they note, “It is unrealistic to believe that 100% of eligible patients will enroll, but even with a 10% enrollment rate, the annual cost to Medicare could reach $3.7 billion — just under 1% of total 2018 Medicare Part A and B expenditures. Additional costs might be accrued as Medicare Advantage and other private payers adopt similar coverage and reimbursement.”
As they emphasize, “Research is urgently needed to elucidate which patients benefit most from RPM services and which devices and specifications provide the highest clinical value. This information will enable professional societies to publish evidence-based guidelines on who should enroll in RPM programs and which devices and support systems should be deployed to maximize the clinical impact of RPM and the collection of health data. Such studies would also provide evidence to enable CMS to set standards for RPM devices to qualify for coverage. Furthermore, private-sector efforts to create transparency regarding the usability, validation, and data-security profiles of biosensors will support clinicians and researchers in technology-adoption decisions.”