Predictive modeling makes radiology management more lean and effective.
Predictive Modeling (PM) has been a boon for healthcare payers in a number of areas while holding great promise in others. When it comes to high-tech imaging, PM’s proven power should be seen in light of the business imperative of cutting costs, as well as a practical reality: Each year more than $16 billion is spent on unnecessary high-tech imaging tests. Payers who do not take steps to eliminate and defuse precursors to problems or problematic events can expect 16 percent annual compounded growth in total radiology costs. As a solution to this challenge, PM has helped payers profile, predict and modify member health, resource allocation and financial risk.
Predictive modeling makes radiology management more lean and effective.
Predictive Modeling (PM) has been a boon for healthcare payers in a number of areas while holding great promise in others. When it comes to high-tech imaging, PM’s proven power should be seen in light of the business imperative of cutting costs, as well as a practical reality: Each year more than $16 billion is spent on unnecessary high-tech imaging tests. Payers who do not take steps to eliminate and defuse precursors to problems or problematic events can expect 16 percent annual compounded growth in total radiology costs. As a solution to this challenge, PM has helped payers profile, predict and modify member health, resource allocation and financial risk.
In a recent study, major healthcare payer organizations identified key business objectives for the next few years as reduction of overall costs, increasing profits, identifying high-risk members and development of quality disease management programs. When asked to identify the most important issues confronting their employer groups, providers and members, 90 percent of respondents identified high costs as the number one issue, with quality concerns coming in a close second at 84 percent.
With profitability and quality at the top of all stakeholders’ lists, healthcare is looking for ways to manage and improve both. PM, which essentially uses the past to manage the present and predict the future, is proving to be one possible solution. Healthcare payers have recently begun using PM to calculate insurance premiums, predict future group/individual medical expenses and set provider reimbursements, as well as identify members with potentially significant future medical expenses. The use of PM to manage healthcare spending is growing as spending accelerates. As a significant portion of accelerated healthcare spending, high-tech imaging also has begun to look to PM.
The High Cost of Imaging
Today, the U.S. conducts about 80 million advanced diagnostic radiology exams each year for an increase of $30 billion in cost over 2000. In 2006, radiology costs were expected to reach $120 billion nationally, while high-tech utilization continues to increase 15 to 20 percent annually. Payers that do not take steps to address rising costs can expect a 16 percent compounded annual growth rate in radiology costs—one of the most significant increases in any healthcare cost. In fact, imaging costs are growing at twice the rate of the cost of prescription drugs and faster than overall healthcare spending, which is rising only 10 percent each year. That is according to the Centers for Medicaid and Medicare Services Office of the Actuary National Health Statistics Group.
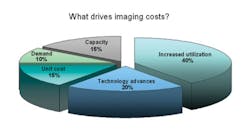
In real numbers, that means a health plan with $12 per member per month (PMPM) cost in 2006 can expect $22 PMPM in 2010 for high-tech imaging procedures. For a plan with 500,000 members, this could mean a total cost increase of $58 million, which begs the question of why this is happening. There are five primary drivers of diagnostic imaging costs:
• Increased utilization. High-tech imaging is no longer science fiction—it’s science fact. As such, today’s tech-savvy physicians use it in medical school and come to rely on it to make—rather than confirm—diagnoses. In this increasingly litigious society, high-tech imaging studies help ensure no diagnostic stone goes unturned. Yet, the more physicians use this high-tech, high-cost equipment, the greater the incidence of redundant studies and false positives that lead to more tests. Moreover, the relative affordability, availability and income potential of imaging equipment has led many physicians to install it in their offices, leading to even more utilization from self-referral.
• Advances in technology. New technologies and new uses of existing technologies will continue to accelerate the pace of innovation in high-tech imaging.
• Increased unit costs.
• Expanded capacity. Equipment availability coupled with a volume-based financial incentive has led to more machines doing more studies.
• Expanded consumer/patient demand. Direct advertising to a technologically aware consumer population has created a demand for and expectation of access to high-tech imaging.
Together, these drivers have created a more than $100 billion industry projected to grow as high as $161 billion by 2008. And, while these high-tech tests account for only 25 percent of all imaging procedures, they are responsible for 75 percent of the inflationary trend. Yet, the real problem is that at least one-third of advanced imaging testing is inappropriate, with more than $16 billion spent on unnecessary radiology tests.
Clearly physicians’ orders drive utilization of high-tech imaging. However, contrary to long-standing industry belief, overutilization of high-tech imaging is not the fault of a few doctors ordering inappropriately all the time. In reality, most physicians order inappropriately some of the time. Therefore, the $16 billion question is when and why does a particular doctor order appropriately or inappropriately? Finding the answer and managing the behavior can mean huge savings.
How PM Works for RM
Long employed in industries from financial services to air traffic control, PM is relatively new to healthcare and even more so to radiology management (RM). The reason for this slow adoption is that predictive models have only recently evolved to the required level of sophistication for healthcare.
First generation models provided a simple form of risk adjustment using basic patient demographic and clinical data such as age, gender and diagnosis, which provided a limited set of variables with limited efficacy. Second generation models used a broader set of member data to characterize members’ conditions. This facilitated development of methodologies that could classify or group patients into risk categories such as Ambulatory Care Groups.
Although they simplified patient analysis and management, these groups were neither specific nor sensitive enough and often led to care that was unnecessary, ineffective or incomplete. Today’s third-generation models employ artificial intelligence (AI), with these models typically falling into one of two categories:
1. Conventional AI models. These models or algorithms, employ formalism and statistical analysis. They operate on the principle that defined inputs to a series of defined steps will follow a defined path to a defined output. At its most basic, a recipe is an example of an algorithm.
2. Computational AI models. These models employ ‘learning’ or iterative development. They use empirical data as an input and change their structures and output based on external or internal information that flows through the network. Neural models are examples of computational systems with very strong pattern recognition capabilities. Thanks to this increased sophistication, PM can now be used to model not only which members will get the most sick, but also which doctors will order which imaging tests to diagnose and treat them.
All RM cost systems employ a sentinel component that saves payers money and improves care by:
• Denying inappropriate (unnecessary) tests. Most systems map ICD9 diagnosis codes against CPT-4 procedure codes, denying them when the former doesn’t support the latter. For example, if a physician ordered a computerized axial tomography scan of the head or brain (CPT-4 code 70450) for a patient diagnosed with a broken ankle (ICD9 code 824.0), the test would be denied.
• Approving a more appropriate test. In this instance, the inappropriate case is denied, but a more appropriate and/or efficacious test is approved. Using the broken ankle example, the physician should initially perform a basic X-ray of the ankle (CPT-4 code 73600), instead of requesting a CT or MRI of the ankle/lower extremity.
• Redirect patients to less expensive delivery locations. Imaging procedures performed in a hospital setting generally cost 100 percent more than those done at a freestanding imaging center. Yet, in the majority of markets nationwide, 60 percent to 70 percent of imaging utilization occurs in a hospital setting. RM systems can automatically suggest alternative, less expensive options to whoever is scheduling the test. The sentinel effect helps payers save current dollars and improve extant care. However, adding a predictive model takes radiology management a step further by providing prescient logic.
Employing a neural PM in RM allows a plan to:
• Identify inappropriate studies more accurately.
With the best neural models, decisions are based not only on CPT-4/ICD9 codes, but also such other factors as a particular patient’s demographics, the physician’s specialty and the physician’s past ordering habits. These additional variables do a more thorough job of identifying both potentially inappropriate and appropriate orders, thereby streamlining and improving the process. In most cases, the plan’s costs go down while quality goes up. In addition, physician satisfaction increases if the RM program rewards consistently appropriate ordering with fast approvals.
• Base approvals on ‘real’ data. Neural models can use experiential data to make predictions and they can analyze more variables. As variables change, the model adapts and provides real-world information. This ‘learned,’ more comprehensive knowledge gives plans a more accurate and comprehensive information base upon which to perform business planning.
• Manage by exception. The smarter the model, the more accurate decisions it can make to approve or deny up front. Only the questionable orders are forwarded for clinical review, or in some cases, review by physician medical directors. This provides the ability to apply valuable clinical decision support resources to the orders and ordering physicians who need them most.
• Adapt to market changes. Having a PM in place allows a plan to adjust the intensity of its utilization management program, thereby narrowing or widening its focus based on plan and market needs.
PM Today and Tomorrow
The advantages of PM for RM are many. However, despite their potential to actually improve the quality of care while reducing costs, the use of neural models for radiology management conjures images of provider profiling and denial of care. Clearly, radiology management with a prior authorization component leads to denied orders. Overutilization of high-tech radiology increases the cost of plans and reduces the quality of care, but proper utilization optimizes both costs and care.
But physicians typically don’t intentionally order inappropriately. The reality is that the changing pace of technology coupled with the increasing demands on a physician’s time make it almost impossible to stay abreast of what’s available and how best to use it. Physicians are human, and the most successful PM deployments for radiology management programs account for that by retaining the human element as part of the process.
Even the most evolved neural models cannot replace the critical thinking of experienced clinicians. Predictive models can successfully guide clinical practice when the variables are clearly defined and demonstrated. Fortunately, this is the case most of the time. However, when there are questions, the most successful radiology management programs forward them to real clinicians—nurses and physicians—to make the final decision about appropriateness. The best RM programs then facilitate peer-to-peer review of cases as needed. The result is that physicians have access to the evidence-based clinical decision support they need to provide the best in patient care.
APRIL 2007