What really happens in the middle of an unfolding natural disaster—as opposed to what people might think might happen? That was question was answered in detail on Wednesday morning at the Florida Health IT Summit, sponsored by Healthcare Innovation, and being held May 21 and 22 at the Saddlebrook Resort in the Tampa suburb of Wesley Chapel. Pamela King, health information technology outreach coordinator Florida’s Agency for Health Care Administration (AHCA), shared with the healthcare leaders gathered, the experience of Hurricane Michael, in the context of health information exchange (HIE) and data-sharing, in a presentation entitled, “How the Florida HIE Helped the Community During Hurricane Michael.”
King began her presentation with a brief overview of the Florida HIE, which she oversees in her position with AHCA, noting that the HIE has developed a federated model without a statewide central data repository. “We allow for services that allow for and promote transportation of data,” including among other elements, “encounter notification service for admits, discharges, and transfers to and from hospitals. We also promote the use of a federated query model service.” As
As of the present moment, the scope of the HIE includes the following elements:
Ø Over 250 hospitals, covering 95 percent of all acute-care and 80 percent of all rehab, hospital beds in Florida, are involved in sharing data via the HIE
Ø 8.8 million of the 22 million lives in Florida are covered by the data exchange
Ø The HIE is delivering over 1 million alerts per month
Ø Data is being sent to hospitals, ambulatory care practices, ACOs, and health plans
Ø The HIE is improving care coordination and transitions of care
Ø It is also reducing hospital admissions and readmissions
Ø It is also supporting value-based payment models
Ø The HIE’s processes facilitate flexibility: users can elect to receive either real-time or batched messages
Hurricane Michael
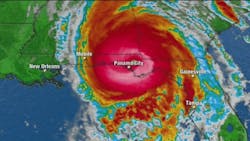
The bulk of King’s presentation on Wednesday was devoted to a discussion of what happened during Hurricane Michael, which hit the Florida panhandle in early October 2018, and in its aftermath.
As the Florida HIE’s website notes in an article on the site, “The Florida Health Information Exchange used the Encounter Notification Service (ENS®) during Hurricane Michael to assist health care providers in locating patients that were displaced due to the storm. Once an emergency was declared for Florida, we paused the routine purge of hospital encounter data flowing into ENS. This resource of encounter information was used post-storm to locate persons who may have been in a hospital or visited an Emergency Department in Florida during the emergency. The Agency for Health Care Administration worked with a large home health agency and several dialysis organizations serving the Panhandle area to help locate their patients. From the pool of patients that couldn’t be located, we were able to identify 348 admissions, discharges or emergency department events for 150 individuals and provide specific encounter information to the requestors.”
As the article goes on to state, “The limited use of ENS as part of Hurricane Michael recovery shows great promise for emergency response in the future. Additional data sources, including long-term and post-acute care facilities, will further enhance the ability to assist vulnerable populations impacted during emergencies. The Florida Health Information Exchange is pleased to be able to provide a service that enables continuity of care for vulnerable Floridians even during a disaster.”
In framing the experience for her audience, Pam King noted on Wednesday that Hurricane Michael had several elements to it that made it particularly devastating to the Florida Panhandle and its residents. For one thing, the forecast had been for a relatively mild hurricane—a category 1 hurricane—but the storm suddenly strengthened dramatically, ultimately becoming a category 5 hurricane, the strongest type. Numerous things happened as a result, King told her audience. Not only were Gulf Coast Regional Hospital’s and Bay Memorial Hospital’s facilities largely destroyed; because the hurricane had wreaked greater damage inland than directly along the coast, people were going to the beaches to get supplies, she noted. “And the roads around Panama City are small two-lane roads, with limited capacity. People couldn’t get out” before the hurricane hit.
Meanwhile, King noted, “We knew where the patients were who were being moved, but the home health and dialysis patients who had stayed in place during the disaster, we didn’t really know what was going on with them. And our HIE does not maintain any data. So when the governor declared a state of emergency, we started maintaining the data, to know where the patients were going, being admitted to. The home health and renal care centers that reached out to us for help to find their patients, we had requests for about 1,000 patients; we found 150 of them through our encounter notification system, because they were admitted into a facility.”
Meanwhile, King said, though absolutely no one had wished for that natural disaster to happen, she and her colleagues all worked in the moment to learn what could and should be done in situations like this one. And in that, she said, “We had a vision of the services we could provide, and this allowed us to learn from this experience—we know disasters are coming.”
Among the biggest lessons learned, King emphasized, was that “this process was very manual.” Crumpling a sheet of paper, she told her audience, “People were hand us crumpled pieces of paper like this, with handwritten information scrawled on them. So we tried to read them as we went looking for people. At AHCA, we were putting in people’s names, and our vendor was taking that information and uploading it, putting it into a format where they could upload and look for people. So there was a lot of room for error in the copying and pasting and retyping processes.”
As a result, King said, “We learned that we needed to automate this entire process. And some of the infrastructure we thought was in place at the Department of health, we found out that they didn’t have the information we thought they had. Because the Department of Health was responsible for ESS 8, which is emergency healthcare. So we’re looking with them at how we can deploy into emergency shelters, and do an ENS emergency census. Are patients in a place where there’s electricity? Do they need to be transported? Those kinds of things. So we’ve been working with the Department of Health into looking at having tablets and cell phones where they could upload patient information, and send that information through our encounter notification service, so that we’d know where a patient is, so when someone is looking for that patient, we know they’re in a special needs shelter, not a hospital, for example. Right now, we only have hospital data; we’re getting SNF [skilled nursing facility] data. But a lot of these patients were at special-needs shelters.”
Given all that, King said, “For this year, we anticipate having the ability to deploy that to our special-needs shelters if there are hurricanes or fires. We’re having fires in the Panhandle because of dried-out timber that’s down. But,” she added, “we know there’s a great value proposition for using the data that we have and the data we can get, for disasters. What information do the emergency management services need as they’re picking up and dropping off patients? We’d like to get the information on the emergency shelters, too.”
In sum, King told the audience, the experience of leveraging HIE-facilitated data during and after a live natural disaster like Hurricane Michael, taught her and her colleagues across healthcare in northwest Florida, many lessons.
Following her presentation, King sat down with Healthcare Innovation Editor-in-Chief Mark Hagland to answer a few questions. Below is their exchange.
Given everything that you and your colleagues learned during and after Hurricane Michael, what should CIOs, CMIOs, and other healthcare IT leaders think about your experiences?
I think that HIT leaders need to look at technology outside of the realm of day-to-day patient care. How can we use HIT when there’s an urgent or emergent need? One of the things is just to think about it. Because one of the things we tend to do as human is to focus on the here and now. And HIT leaders have so much to do, but in a second, you’re here-and-now could be destroyed. It could be an earthquake, a fire, tornados. So no matter where we’re at, it’s having a plan in the place, and having conversations about what do we do “IF”? And a lot of times, it’s the CEO and c-suite who need to be thinking of what might happen in different scenarios. What if we were inundated with patients from other places? Often, hospital leaders think about destruction to their own facilities, but not about surges of patient volume coming from facilities that have been destroyed or damaged.
Obviously, that’s where health information exchange can really demonstrate its value.
Yes, absolutely; if we’re inundated with patients, I need information about those patients, and so I need to get the data on those patients, and HIE promotes that. Because if I’m getting a patient in cold, I won’t know everything I need to know. And maybe this person just had a surgery in the middle of a hurricane, and they’re being transported fast, and there’s no data being shared between people, so you need the data to be shared between systems.
Meanwhile, those entities being damaged, have repetitive servers somewhere, and need to be able to share data from their servers with other facilities and organizations. In this case, a lot of patients were being sent to rural hospitals, and needed to be stabilized, etc. And being able to send information—OK, I’m going from this hospital that’s been destroyed to a smaller, critical access hospital, and now I’m being sent on to a larger hospital, and so that’s two jumps, and you have data now from two different places; so having that information and being to share it, is very important. Usually, the patients can’t share the information, and often, the family members aren’t riding with them. So it’s important we have a system in place that can facilitate the data following the patients.